Toxicity Studies in Vaccine Clinical Development and Registration

Complete the form below to unlock access to ALL audio articles.
Before the safety and efficacy of a new vaccine can be evaluated in a Phase I clinical trial with human subjects, it must first undergo non-clinical safety evaluation in animal models. Regulatory Agencies such as EMA, FDA, PMDA, MHRA, Health Canada and many others require that the safety studies performed prior to Phase 1 must be conducted under Good Laboratory Practice (GLP) standards.1 Additional nonclinical safety studies are required during the clinical development process and are normally submitted as part of the registration dossier for the vaccine. In addition, specific additional nonclinical safety studies are needed for adjuvants and immunostimulants.
Global regulatory framework
The principal regulatory guidance for nonclinical studies, including toxicology, is listed below in Table 1.
Table 1. The principal regulatory guidance for nonclinical studies.
| Agency | Title | Year |
| WHO | Guidelines on Nonclinical Evaluation of Vaccines | 2005 |
| WHO | Guidelines on the Nonclinical Evaluation of Vaccine Adjuvants and Adjuvanted Vaccines | 2013 |
| EMA | Note for Guidance on Preclinical Pharmacological and Toxicological Testing of Vaccines | 1995 |
| EMA | Guideline on Adjuvants in Vaccines for Human Use | 2005 |
| FDA | Guidance for Industry: Considerations for Developmental Toxicity Studies for Preventive and Therapeutic Vaccines for Infectious Disease Indications | 2006 |
| FDA | Guidance for Industry: Preclinical Assessment of Investigational Cellular and Gene Therapy Products | 2013 |
| SFDA China | General Principles of Technical Review in Preclinical Safety Evaluation on Preventive Biological Products, GPT2-1 | 2005 |
| MHLW Japan | Guideline for Non-clinical Studies of Vaccines for Preventing Infectious Diseases | 2010 |
The first regulatory agency guidance specific to vaccine non-clinical safety studies was issued by EMEA (precursor to EMA) in 1995, illustrating that vaccine nonclinical safety evaluation is relatively new field, compared with the non-clinical toxicology studies for other categories of pharmaceutical products or chemicals. The scope of these guidance documents includes preventive and therapeutic vaccines and adjuvants. A wide range of vaccine types are covered, such as polysaccharide vaccines, recombinant protein vaccines, live or inactivated viral vaccines, protein (toxoid) vaccines and DNA/RNA vaccines.
Since many modern vaccines are adjuvanted, the most relevant and widely applicable guidance listed in Table 1 is WHO´s 2013 Guidelines on the Nonclinical Evaluation of Vaccine Adjuvants and Adjuvanted Vaccines. This publication is intended to facilitate consistent and harmonized international regulatory expectations for adjuvants and adjuvanted vaccines to national regulatory authorities (NRA) as well as vaccine manufacturers. In addition to nonclinical safety assessment, the areas covered also include manufacturing and quality, preclinical immunology, first time in human clinical trials and classification of adjuvants. The WHO guidance makes a distinction between “novel” and “new” adjuvants.
What is a novel adjuvant?
A novel adjuvant is one that has not been included in a licensed vaccine.
What is a new adjuvant?
A new adjuvanted vaccine includes unlicensed adjuvanted vaccines along with previously licensed products with significant changes in the antigen and/or adjuvant production process, major formulation changes (such as a change in adjuvant or addition or removal of one of the components) or a new route of administration.
General considerations for vaccine toxicity assessment
Vaccines are a complex, diverse class of biological products, in which the vaccine formulation is not the final triggering component and elements of the immune system are the effectors. Consequently, vaccine nonclinical safety studies must be designed to assess the inherent toxicity of the vaccine, toxicity of impurities, contaminants and/or excipients, toxicity due to interaction of formulation components as well as toxicity linked to the immune response.
Considerations for animal models used in vaccine toxicity studies include:
- The relevance of animal model
- Demonstration of an immune (immunogenic) response
- Sensitivity of the model for the detection of immune-mediated effects or intrinsic toxicity
- Value of the historical control database for a specific species/strain and the consistency of effects with the clinical safety data
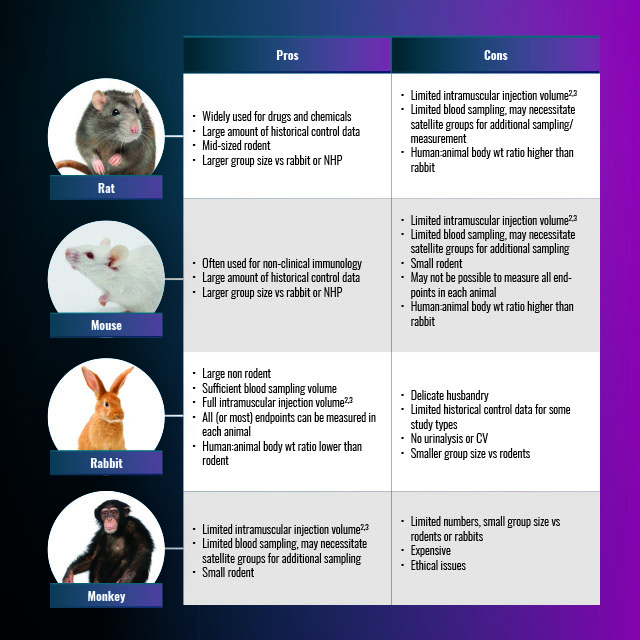
Although the WHO 2013 guidance indicates that toxicity studies in a single species relevant for the vaccine is sufficient, some NRAs may require toxicity studies in more than one species. The most widely used species for vaccine GLP toxicity investigations are rats, rabbits, mice and non-human primates. The pros and cons of each are summarized below in Table 2.
Table 2. The pros and cons of rat, rabbit, monkey and mouse models for toxicity studies.
Study types and designs
The principal types of toxicity studies required for adjuvanted vaccines and adjuvants/ immunostimulants during vaccine clinical development are summarized below:
- Single dose – local tolerance
Pre-phase 1 (GLP)
- Local tolerance
- Single dose toxicity (usually combined with local tolerance)
- Repeated dose toxicity
- Safety pharmacology (adjuvant systems and immunostimulants)
- Genetic toxicology (immunostimulants)
Phase 1-3 (GLP)
- Repeated dose toxicity studies (supporting CMC changes)
- Reproductive toxicity studies (prior to or in parallel with Phase 3)
- Mechanistic studies (if required)
For GLP toxicity studies, regulatory guidance requires that the item should be the final formulation of the vaccine to be used in the clinical trial, or a lot equivalent to the GMP clinical lot. The characterization of the lot to be used in GLP studies includes the identity, concentration, purity (residual cellular DNA, RNA and protein), potency, stability, sterility and adventitious agent testing.
(i) Single dose toxicity and local tolerance
The WHO guideline indicates that local tolerance can be combined with a single dose or repeated dose toxicity study. The rabbit is often used, since it can be injected intramuscularly with the full human dose in a single site.2,3 The dose to be used is the full human dose (rabbit) or a fraction of the full human dose (rodent). Toxicity parameters measured include mortality, clinical signs and body weight gain. Local reactogenicity is scored according to for erythema and oedema 0, 3, 24, 48, and 72h post-injection.4 Post-mortem analyses include gross necropsy including the injection site, gross observations of major organs and histological assessment of injection site.
(ii) Repeated dose toxicity
The purpose of this study is to identify and characterize the potential toxic effects of repeated administration of a vaccine formulation intended for human clinical trial and eventual registration.
Parameters to be considered when planning this study include the animal species/strain, the clinical plan, dosage form, dose, and route of exposure, frequency of human exposure, the device for administration and any previous data available for the same (or similar) formulation. The study is performed via the intended route of clinical administration. The dosing schedule is similar to the human schedule in terms of the number of injections administered, but not the interval between the doses. In order to maximize vaccine exposure, one additional injection is given compared with the human schedule. Therefore, a vaccine with a human clinical schedule of two doses would normally be supported by a three-dose toxicity study. Animals in this study are divided into two necropsy time points following the last injection, early (three days post last dose) and late (four to 13 weeks post last dose), the latter intended to assess the reversibility of findings and/or delayed effects.
Measurements taken during the study include:
- Clinical signs daily
- Body weights
- Food consumption
- Body temperature on several occasions after the first and subsequent doses
- Ophthalmology
- Clinical pathology (hematology, biochemistry) post first and last injection and at necropsy
- Acute phase proteins (C- reactive protein, which was added as an inflammatory biomarker in 2013 WHO guideline)
- Gross necropsy examination
- Injection site histopathology
- Organ weights
- Histopathological examination of a full panel of tissues/organs as specified in the 2013 WHO guideline and serology to assess vaccine exposure.
(iii) Pre-, peri- and post-natal reproductive/ developmental toxicity
A reproductive/developmental toxicity study is required pre-licensure if the vaccine is intended for administration to women of child-bearing potential. This study is normally conducted prior to, or concurrently with, Phase III, and included in the licensing application. The most detailed guidance for this study type is provided in the FDA 2006 guidance.5 The recommended design is a combined developmental, peri- and post-natal study and the species most often used are the rat or rabbit. An example of a typical rat study design is shown in Figure 1 and described in Barrow, and Segal et al.6,7 Immunogenicity assessments in dams, pups and foetuses are required to confirm vaccine exposure. Each test group is subdivided into a caesarean and littering phase, the former for assessment of foetal development and the latter for assessment of potential postnatal effects up to weaning.Typically, one- two injections are given to females prior to mating with untreated males, and several additional doses are given to females during gestation. A further dose is given to females during the lactation phase.
 Figure 1. A typical rat study design.
Figure 1. A typical rat study design.
Female fertility is part of the standard reproductive toxicity study design. The assessment of male fertility is not normally required in vaccine reproductive toxicity studies according to FDA’s 2006 Guidance.
However, the WHO 2005 Guidelines provides no specific exemption for male fertility studies, and states that the need to conduct fertility assessments should be considered on a case-by-case basis. The need for the assessment of potential vaccine effects on male fertility is based on the frequency of administration, number and the age of male subjects to be exposed in Phase III and during eventual commercialization, and whether the antigen is expressed in male reproductive tissues.
Requirements for adjuvants
Vaccine adjuvants are considered a new additive to be administered to humans, with testing adapted to the vaccine environment. In this context an immunostimulant is defined as an individual substance used in conjunction with a vaccine antigen to enhance the immune response to the antigen, while an adjuvant system (AS) is a combination of immunostimulants. Toxicity testing of adjuvants is intended to discriminate potential effects seen in final vaccine and to establish a safety package for the AS and/or immunostimulants to be used in various human vaccines. The following studies should be performed with the immunostimulant alone:
- Single dose toxicity and local tolerance
- Repeated dose toxicity
- Pre- and postnatal reproductive toxicity
- Genotoxicity studies in accordance with ICH S2
- in vitro Ames mutagenicity test (OECD 2020)
- in vitro clastogenicity test (OECD 2016a; OECD 2016b)
- A micronucleus test in vivo (OECD 2016c)
When a new AS is proposed for use, toxicological information can be obtained by including an "AS group" in the vaccine toxicology studies (control group; AS group; vaccine group). The timing for AS toxicology studies would then follow that for the vaccine formulation, as described previously.8,9,10,11
An evolving area
As can be seen from Table 1, the nonclinical safety evaluation of vaccines is an evolving area, and vaccines face an increasing number of regulatory guidelines. The 2013 WHO Guideline provides consistent and harmonized international regulatory expectations for adjuvants and adjuvanted vaccines. Nonetheless, nonclinical testing required for adjuvants and adjuvanted vaccines needs to be examined on a case-by-case basis.
References:
1. OECD. Principles on Good Laboratory Practice: Paris, 1998. https://www.oecd.org/officialdocuments/publicdisplaydocumentpdf/?cote=env/mc/chem(98)17&doclanguage=en. Accessed May 10 2021.
2. Diehl K, Hull R, Morton D, et al. A Good Practice Guide to the Administration of Substances and Removal of Blood, Including Routes and Volumes J. Appl. Toxicol. 2001. doi:10.1002/jat.727.
3. Recommended Dose Volumes for Common Laboratory Animals. IQ 3Rs Leadership Group - Contract Research Organization Working Grouphttps://iqconsortium.org/images/LG-3Rs/IQ-CRO_Recommended_Dose_Volumes_for_Common_Laboratory_Animals_June_2016_(2).pdf. 2016. Accessed May 10 2021.
4. OECD Guideline for Testing of Chemicals. OECD. https://www.oecd-ilibrary.org/docserver/9789264242678-en.pdf?expires=1620655074&id=id&accname=guest&checksum=C9A661DB7E553AF3F2C3A9220F76C4AB. 2015. Accessed May 10 2021.
5. FDA. Guidance for Industry: Considerations for Developmental Toxicity Studies for Preventive and Therapeutic Vaccines for Infectious Disease Indications Center for Biologics Evaluation and Research. 2006. https://www.fda.gov/media/73986/download. Accessed May 10 2021.
6. Barrow P. Developmental and reproductive toxicity testing of vaccines. J Pharmacol Toxicol Methods. 2012;65(2):58-63. doi:10.1016/j.vascn.2011.12.001.
7. Segal L, Thacker K, Fochesato M, Giordano G, Garçon N, Destexhe E. Intramuscularly administered herpes zoster subunit vaccine has no effects on fertility, pre- and post-natal development in Sprague-Dawley rats. Reprod Toxicol. 2017;69:297-307. doi:10.1016/j.reprotox.2017.03.015.
8. OECD. Test Guideline No. 471. Bacterial Reverse Mutation Test. OECD Paris, France. 2020. https://doi.org/10.1787/20745788. Accessed May 10 2021.
9. OECD. Test Guideline No. 476. In Vitro Mammalian Cell Gene Mutation Tests using the Hprt and xprt genes. OECD Paris, France. 2016, OECD Paris. https://doi.org/10.1787/20745788. Accessed May 10 2021.
10. OECD. Test Guideline No. 473. In Vitro Mammalian Chromosomal Aberration Test. OECD Paris, France. 2016. https://doi.org/10.1787/20745788. Accessed May 10 2021.
11. OECD. Test Guideline No. 474. Mammalian Erythrocyte Micronucleus Test. OECD Paris, France. 2014. https://doi.org/10.1787/9789264224292-en. Accessed May 10 2021.



